Thermography & Arthritis
This Photo by Unknown Author is licensed under CC BY-SA
Can Thermal Scans Detect the Early Onset of Arthritis?
In 2020, the CDC (Centers for Disease Control and Prevention) estimated that 54.4 million American adults (22.7%) suffer from arthritis, a figure that is projected to rise to 72 million by 2030 (according to the World Health Organization). Clinicians confirm that early diagnosis of the disease remains key because identifying and treating the disease at the earliest possible stages can significantly limit the degeneration of joints caused by the disease, thereby maximizing the quality of life for the patient.
Incredibly, thermography (specifically, IRT, or Infrared Thermography) offers impressive benefits in the early detection and treatment of osteo-, rheumatoid, and other forms, of arthritis (such as juvenile arthritis, which affects children).
Let’s takes a look at this innovative, pain-free, non-invasive technology to see exactly how effective and powerful it can be in fighting this debilitating disease.
Arthritis: A Snapshot
A significant number of Americans – over 54 million – currently suffer from arthritis. Whilst this figure represents the highest ever recorded prevalence of the disease, the CDC still counsels that this number is set to rise significantly over the next few years. Concerningly, the disease, previously associated with aging adults, seems to have the capacity to strike at any point in the life span, with around 60% of arthritis sufferers still under the age of 65.
Critically, the CDC also reports that cases, where arthritis has severely limited day-to-day activities, has risen by 20% in the last twenty years, suggesting a higher level of severity of the disease, with around 24 million sufferers now reporting a meaningful impact on their ability to undertake normal daily activities. Direct medical expenses attributed to arthritis cost an estimated $81 billion a year.
Clearly, there has never been a more urgent need to engage with technologies, such as IRT, that significantly improve our ability to spot arthritis at its earliest stages. So let’s find out a little more about how IRT might prove so valuable in the fight against arthritis.
Hidden
What is Arthritis, Exactly?
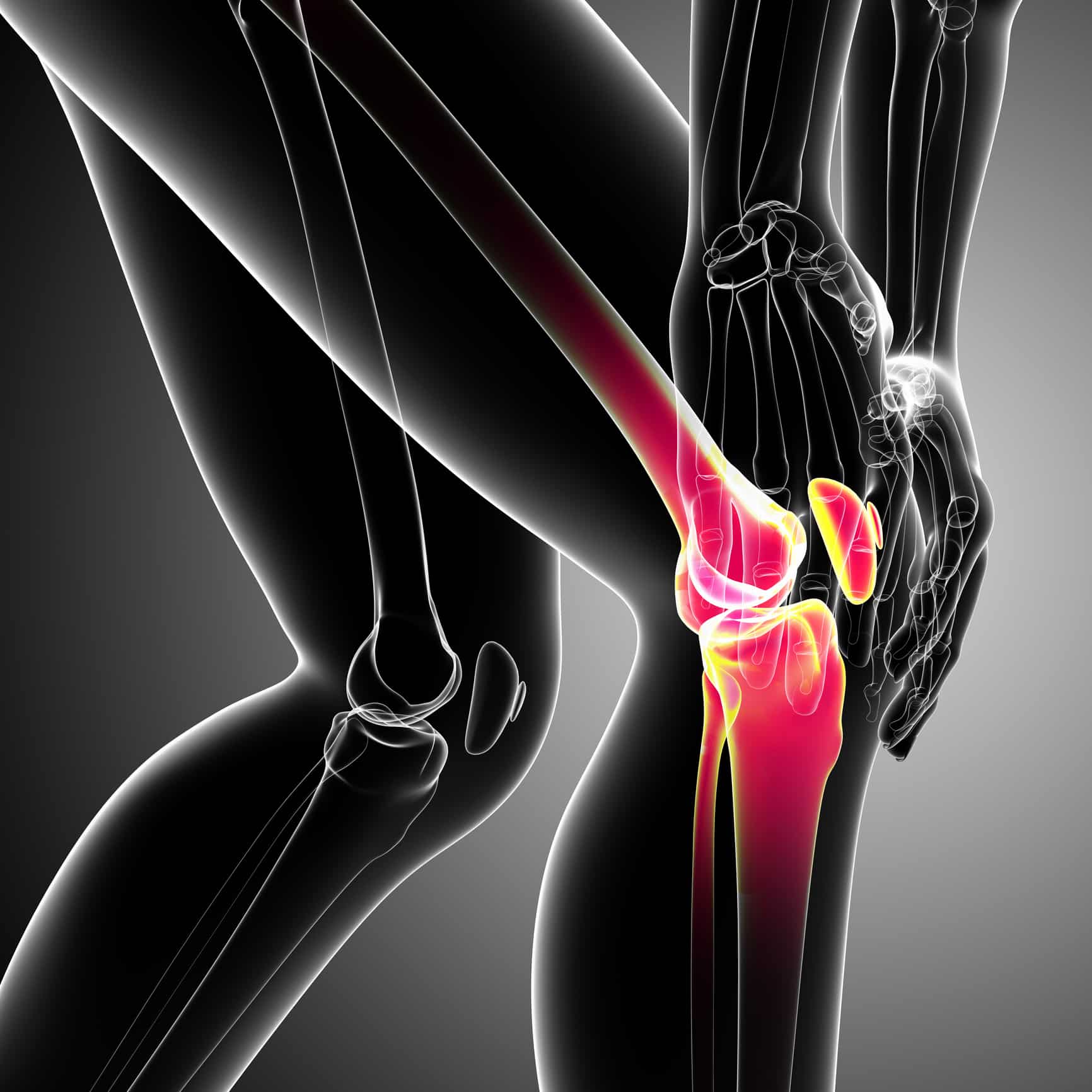
Arthritis encapsulates several distinct pathologies, although all share the same main character of the loss of cartilage in synovial joints, usually accompanied by inflammation, pain, and swelling. The most common and well-known types of arthritis are osteoarthritis, a degenerative joint disease, and rheumatoid arthritis, a systemic autoimmune, inflammatory disorder. Arthritis patients are most likely to report pain in their hands, hips, knees, and feet.
Thermography: Advancing Head & Neck Care
One specific area of the body for which thermography – a test that relies on heat – has proven powerful is in the head & neck region, partially because ‘the human body is considered to be a stairway of heat with the highest temperature in the forehead and cervical regions’.
Subsequently, the efficacy of thermal imaging techniques in the early treatment of cerebrovascular disease, oral inflammation, thyroid dysfunction, periodontal disease, face & mouth cancer (including cervical lymph node metastasis and oral cancer) has emerged with strength in recent years.
How does IR (Infrared Thermography) Work?
Infrared thermal imaging (IR) is a kind of functional imaging that provides a highly effective, non-invasive, and dynamic measure of heat radiated from the superficial dermal microcirculation of our skin (approximately 1–2 mm below our epidermal surface). As the temperature and microcirculation of our skin is influenced significantly by inflammatory, metabolic, and toxic factors, many pathological processes (such as arthritis) manifest as local changes in epidermal heat and blood flow.
Why are these facts so relevant in the context of IRT, and how can they help clinicians with the early diagnosis of arthritis?
Well, IRT measures patterns of blood flow and conductive transfer of heat near the surface of our skin, reflecting thermal processes that are taking place deep in the body. Any unusual disturbances or anomalies show up in IRT scans, which can immediately warn a clinician of the presence of arthritis well before any joint damage has taken place.
Can I Trust Infrared Thermography?
Yes, you can. Infrared thermal imaging has been clinically tested and utilized in the context of the study of many rheumatological conditions, including Raynaud’s phenomenon (a circulatory disorder that can make the patients’ extremities extremely cold and painful), scleroderma (an immunological disorder causing thickening of the skin), reflex sympathetic dystrophy (a form of CRPS – Complex Regional Pain Syndrome), hand and knee osteoarthritis, rheumatoid arthritis (RA), juvenile idiopathic arthritis, and in the monitoring of the effectiveness of anti-inflammatory arthritis therapies.
Let’s take a look at the use of IRT in two of the most common forms of arthritis: osteoarthritis (OA) and rheumatoid arthritis (RA) to find out more.
IRT & Rheumatoid Arthritis (RA)
In the case of osteoarthritis (OA), joint cartilage breaks down over time over time, affecting the smooth cartilage lining of the joint. Once the cartilage lining starts to roughen and become thinner, surrounding tendons and ligaments need to work harder to compensate, causing swelling and the formation of osteophytes (bony spurs).
The resulting severe loss of cartilage (which usually affects the hands, knees, hips, and spine) can cause bones to rub together, leading to significant pain and alteration of the shape of the joint, & forcing bones out of their usual position. The disease can ultimately lead to severe deformity and disability if left untreated. Early IRT scans can identify significant adaptations in heat and blood flow that can indicate arthritis, allowing the clinician to treat the condition before any joint damage has occurred.
IRT has been extensively studied in clinical environments across the world, confirming the powerful relationship that exists between skin temperature at the ROI (the region of interest, e.g., osteoarthritic knee) and the presence and progression of arthritis.
A recent (2010) Duke University study of thirty osteoarthritic and non-osteoarthritic women, for example, reported an association between the temperature of the skin surrounding the knee joint (the joint cutaneous temperature at the patellar) with the severity of osteoarthritis, as measured by X-ray. Similarly, a recent (2012) 22-patient study of the use of IRT in the detection of osteoarthritis of the knee, performed at LACM (Laboratory of Mechanical Stresses Analysis) and the University of Reims Champagne Ardennes, confirmed that infra-red thermography can successfully highlight thermal asymmetries, and that surface skin temperature can be used as a key parameter in the evaluation of pain.
Another recent study performed at Mahidol University in 2017 in Thailand reported significant differences in the mean and maximum temperatures assessed by IRT as mediated by the severity of arthritis suffered by the patient.
A clear relationship was also shown between the subjective assessments of pain intensity provided by young children with juvenile arthritis and joint temperature.
IRT & Rheumatoid Arthritis (RA)
IRT has also proven significantly successful in screening for RA. Rheumatoid arthritis (RA) is an autoimmune systemic connective tissue disease that often begins around the ages of 40-50 years of age but often progresses unnoticed until painful physical symptoms begin to manifest.
In RA, our immune system cells attack healthy cells, causing inflammation and the degeneration of joints. This in turn leads to significant pain and loss of mobility in the sufferer and can also lead to the development of problems with other bodily tissues and organs. It is characterized by inflammation, tenderness, and swelling in the synovium (outer covering) of the joints, adaptations in the shape of a joint, the wearing down on bone and cartilage, and even the destruction of the synovial joint itself.
Around 90% of RA patients complain of pain in the feet, where swelling and hypertrophy of the synovial membrane of the joint can lead to painful structural changes and deformities (e.g., valgus alignment of the rear foot, or toe deformities).
Whilst X-ray, MRIs (magnetic resonance imaging), and other imaging techniques identify structural changes caused by RA, they cannot pick up on the minute changes in superficial (skin-level) dermal macro-circulation, blood flow, and temperature of a joint that occur earlier in the pathology of the disease.
Conversely, IRT allows a clinician to observe pathological changes in the heat radiation of deeper tissues and organs that radiate to the surface, e.g., at the knee joint, facilitating one of the earliest indicators of arthritis possible, and enabling the clinician to intervene before tissue damage has taken place.
Imagine, for example, an active woman in her mid-40’s, who has experienced a little discomfort in the big toe of her right foot, which she dismisses as an annoying niggle, probably, she thinks, a result of repeatedly wearing high heels at work, or too much road running at weekends.
She is, in fact, experiencing the earliest symptoms of rheumatoid arthritis which could progress, if left unchecked, to advanced joint destruction, severely impacting the quality of her life. Yet she does nothing about it, and the disease progresses further. Routine IRT scans used at this early stage would alert a clinician to temperature and blood flow anomalies in her foot (e.g., an increased temperature, indicative of inflammation, or a decreased temperature, indicative of nociceptive differentiation), maximizing the effectiveness of her treatment plan.
Why is Early Screening so Critical?
The earlier arthritis is picked up, the earlier it can be treated. The quicker the disease is halted in its tracks, the less damage it can cause to joints, leading to less pain, and greater sustained mobility, in the patient.
Subsequently, anyone, but particularly high-risk groups (i.e., women with a family history of arthritis) would benefit from the use of IRT in early, routine screening for arthritis. As a patient does not usually seek help until they experience physical symptoms – pain, discomfort, or swelling, for example – inflammation and joint damage may have already occurred.
Diagnosing arthritis using IRT – before the painful accumulation of fluid, inflammation, increase in blood flow, swelling, heat, redness, and pain are experienced – offers a powerful opportunity to minimize damage caused by the disease, so that the patient receives the best prognosis possible.
Monitoring Arthritis Treatment Interventions
IRT has also proven useful in the monitoring of the effectiveness of arthritis treatments, such as laser treatments, medical acupuncture, and specific medication. In a recent 2017 Hungarian study, for example, the efficacy of low-level laser treatment for osteopathic patients in relieving pain was successfully measured (before, during, and after the procedure), using IRT, where skin temperature readings were used to ascertain the degree of pain relief experienced by the patient.
In another example, a 5-week study published in the Journal of Basic Clinical Physiological Pharmacology assessed the effectiveness of hyaluronic acid solution (1%) in the reduction of pain for post-surgery osteoarthritic patients. Using IRT, researchers recorded localized skin temperature readings and compared these with subjective pain assessments of the patients to reliably conclude the effectiveness of hyaluronic acid in post-surgical pain reduction.
IRT has even been used in multiple studies of the efficacy of bee venom treatment (BVA) on arthritis!
Related Blogs
The Studio Method: Unraveling the Root Cause for Optimal Wellness
The Lifelong Athlete: Longevity Strategies for Peak Performance. Learn about cutting-edge interventions from Doctors Studio in Boca Raton.
Join the Wellness Revolution: Membership Benefits at Doctors Studio
Explore Doctors Studio's unparalleled membership benefits in Boca Raton—top professionals, exclusive discounts, holistic services for a wellness journey
The Five Root Causes Of Insomnia
What are the five root causes of insomnia? Find the root cause of your insomnia and get a full night's sleep—naturally.
Enlarged Prostate In Boca Raton: Treatment And Advice
How to find lasting treatment and genuine empowerment for an enlarged prostate in Boca Raton.
Should You Use Functional Medicine Telehealth Services?
Have you wondered if functional medicine via telehealth is a good fit for you? Learn more today!
What are Symptoms of Non-Celiac Gluten Intolerance?
An undiagnosed gluten intolerance can be a miserable experience.
Pro-Active Health: Is Mold Causing Inflammation?
Is mold causing inflammation? Florida is notorious for mold problems; here’s what you need to know to take charge of your health.
How to Find a Great Functional Medicine Doctor in Boca Raton
Functional medicine is a patient-focused, whole-body approach to healthcare. It is vastly different from the traditional approach that most of us are used to and centers around total wellness, preventative care, and treating or reversing chronic conditions.
Boost Immunity AND Burn Fat? LIPO-MIC: The Gift that Keeps on Giving!
Boost immunity AND burn fat with the ultimate Santa's little helper this holiday season! Lipo-Mic - the gift that keeps on giving!
Is Non-Celiac Gluten Sensitivity Making You Ill?
What is Non-Celiac Gluten Sensitivity? And is it responsible for your digestive and health problems? Read on to find out!










