Compounded Sex Medications in Boca Raton, FL
Compounding Means Created Uniquely For You
Doctors Studio is committed to providing highly individualized care to each and every one of our patients.
Therefore, solutions to symptoms are carefully designed SPECIFICALLY for each person. As these combinations (and dosages) are not available commercially (the combinations are too specific), many of our medical solutions come from a highly trusted and reputable compounding pharmacy.
For those unfamiliar with compounding, we hope the following information will be useful.
Let’s see what the American Pharmacists Association can teach us about how compounding works and why it’s used
Frequently Asked Questions About Pharmaceutical Compounding
What is compounding, and why is it necessary?
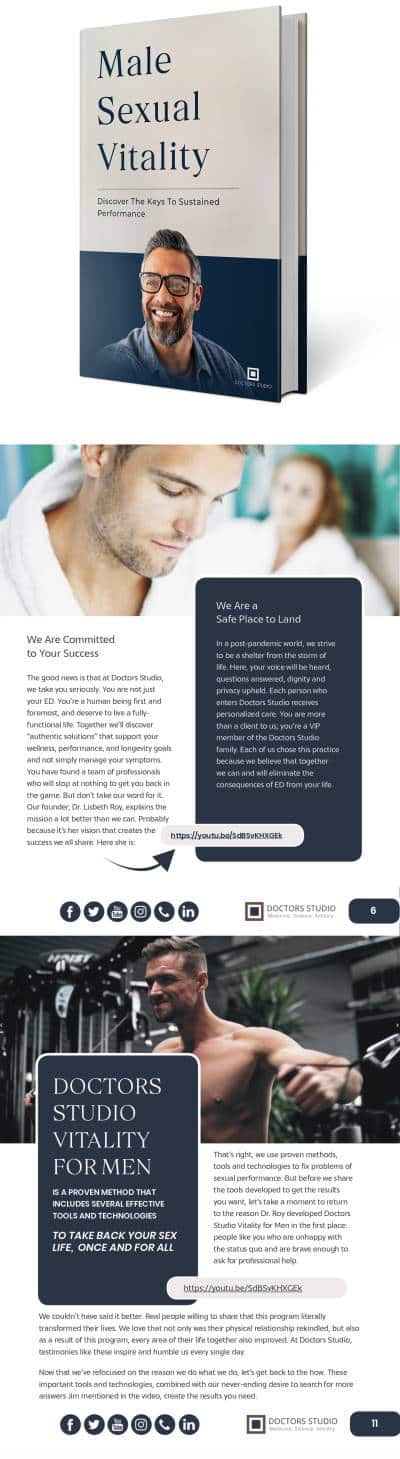
Compounding is the creation of a pharmaceutical preparation—a drug—by a licensed pharmacist to meet the unique needs of an individual patient (either human or animal) when a commercially available drug does not meet those needs.
For instance, a patient:
- May not be able to tolerate the commercially available drug
- The exact preparation needed may not be commercially available
- A patient may require a drug that is currently in shortage or discontinued
The U.S. Pharmacopeial Convention (USP) formally defines compounding as “the preparation, mixing, assembling, altering, packaging, and labeling of a drug, drug-delivery device, or device in accordance with a licensed practitioner’s prescription, medication order, or initiative based on the practitioner/patient/ pharmacist/compounder relationship in the course of professional practice.”
Following are a few examples of how a compounding pharmacist can customize medications based upon a doctor’s prescription to meet a patient’s needs:
- Customize strength or dosage.
- Flavor a medication (to make it more palatable for a child or a pet).
- Reformulate the drug to exclude an unwanted, non essential ingredient, such as lactose, gluten, or a dye to which a patient is allergic.
- Change the form of the medication for patients who, for example, have difficulty swallowing or experience stomach upset when taking oral medication.
Compounding pharmacists can put drugs into specially flavored liquids, topical creams, transdermal gels, suppositories, or other dosage forms suitable for patients’ unique needs. Compounding does not include making copies of commercially available drug products, as this is not allowed by law.
How is pharmaceutical compounding different from drug manufacturing?
Traditional compounding is the preparation of a medication to meet the prescriber’s exact specifications and to be dispensed directly to the patient, pursuant to a valid prescription for that patient. Pharmaceutical compounding is performed or supervised by a pharmacist licensed by a state board of pharmacy. Manufacturing is the mass production of drug products that have been approved by the Food and Drug Administration (FDA). These products are sold to pharmacies, health care practitioners, or others who are authorized under state and federal law to resell them.
What is a compounding pharmacy?
While most pharmacies offer some level of compounding, most compounding is done in pharmacies that have made the investment in equipment and training to do so safely and efficiently. The preparations offered by these compounding pharmacies can be nonsterile (ointments, creams, liquids, or capsules that are used in areas of the body where absolute sterility is not necessary) or sterile (usually intended for the eye, or injection into body tissues or the blood).
All licensed pharmacists learn during their training and education to perform basic compounding. In addition, most pharmacies have some compounding tools, such as a mortar and pestle for grinding materials, graduated cylinders for measuring liquids, balances for weighing solids, spatulas for mixing materials, and ointment slabs on which to work. With such tools and through applying their knowledge, all pharmacists routinely prepare non sterile compounded preparations when requested by prescribers.
Of the approximately 56,000 community-based pharmacies in the United States, about 7,500 pharmacies specialize in compounding services. This means the pharmacists in those facilities spend most or all of their time compounding special preparations for patients. Preparations made in these pharmacies are more likely to include both sterile and nonsterile dosage forms. Compounding also takes place in hospital pharmacies and at other health care facilities.
Who regulates compounding pharmacies? Do compounding pharmacies follow the same regulations as drug manufacturers? Why or why not?
The practice of compounding is regulated by state boards of pharmacy. Community and hospital compounding pharmacists are allowed exemptions to the Federal Food, Drug, and Cosmetic Act of 1938 if they comply with the regulations outlined in Section 503A. All pharmacists and pharmacies engaged in compounding are subject to oversight by both federal and state authorities.
Pharmacists engaged in compounding are expected to follow applicable standards and regulations for the types of preparations that are compounded. FDA has oversight for the integrity and safety of the drugs (called Active Pharmaceutical Ingredients, or APIs, by FDA) used in compounded preparations. The Drug Enforcement Administration (DEA) has oversight for any controlled substances used in the preparation of compounded medications. Controlled substances include narcotics such as hydrocodone, amphetamines, and similar drugs, and drugs such as those used for anxiety and sleep disorders.
In addition, the United States Pharmacopeial (USP) Convention issues standards that apply to compounding. This private, nonprofit organization defines the chemical purity of drugs and also issues practice standards. USP develops standards for the identity, quality, strength, and purity of medicines, dietary supplements, and food ingredients that may be used in compounding preparations. These standards in particular are relevant to compounding pharmacists.
USP General Chapter <797> is a national standard for the process, testing, and verification of any compounded sterile preparations. It provides guidance on preventing microbial contamination and other variances in compounded sterile preparations, regardless of setting (e.g., hospitals, community pharmacies) or who is performing the compounding (pharmacists, nurses, pharmacy technicians, or others).
Compliance with these and other USP guidelines is considered the minimum standard of practice in pharmacy.
Pharmacy Compounding Accreditation
Pharmacy Compounding Accreditation is a service of the Accreditation Council for Health Care (ACHC) that assesses the nonsterile and sterile pharmacy compounding process as defined by a specific set of standards that concentrate on the quality and consistency of medications produced.
How would patients know if their medication is compounded? Knowing that, should they take any precautions, or do anything differently?
Ask. A patient can receive compounded drugs from a typical community pharmacy or a specialty compounding pharmacy, or compounded drugs can be administered by doctors or other health professionals in clinics or medical offices. Patients should ask the person administering a medication or the pharmacist dispensing a prescription whether it was prepared in a compounding pharmacy or manufactured by a drug company. A widely accepted standard of practice is to label all compounded preparations with information stating the medication has been “compounded.”
Does a compounding pharmacist have special training?
Compounding is a central activity to the practice of pharmacy. Pharmacists are taught in pharmacy school how to properly compound medications, and many states test pharmacists’ compounding knowledge and skills before issuing them a license.
Pharmacists who practice in the 7,500 pharmacies that specialize in compounding services have generally had advanced training in compounding after they graduated from pharmacy school. No state currently requires a particular type of training, and no nationally recognized specialty exists for pharmaceutical compounding. Specialized training in pharmacy compounding processes is available through several of the active pharmaceutical ingredient (API) suppliers serving the needs of the compounding pharmacy community.
When is a compounding pharmacy necessary?
A health care provider will prescribe a compounded drug only when commercially available drug products do not meet your needs. If you do not understand why you have been prescribed a special formulation, ask your prescriber. If you are concerned about taking a compounded drug and you and your prescriber agree that you can tolerate the commercially available drug, you may also ask if there is any evidence that your outcome will be better on the compounded formulation.
There are Innovative, Effective,
Solutions for Your ED!
Related Blogs
Aging Backwards: The Science of Age Reversal and Longevity
The Lifelong Athlete: Longevity Strategies for Peak Performance. Learn about cutting-edge interventions from Doctors Studio in Boca Raton.
The Power of Transfer Factors in Functional Medicine
The Lifelong Athlete: Longevity Strategies for Peak Performance. Learn about cutting-edge interventions from Doctors Studio in Boca Raton.
Youthful Aging: Eliminating Senescent Cells for Improved Health
The Lifelong Athlete: Longevity Strategies for Peak Performance. Learn about cutting-edge interventions from Doctors Studio in Boca Raton.
Join the Wellness Revolution: Membership Benefits at Doctors Studio
Explore Doctors Studio's unparalleled membership benefits in Boca Raton—top professionals, exclusive discounts, holistic services for a wellness journey
The Lifelong Athlete: Longevity Strategies for Peak Performance
The Lifelong Athlete: Longevity Strategies for Peak Performance. Learn about cutting-edge interventions from Doctors Studio in Boca Raton.
Is A Functional Medicine Doctor A Licensed Medical Practitioner?
Are you looking for high-quality health care and want to know whether a functional medicine doctor is the right fit? Learn more about credentials here.
Senolytics: The Secret To Reversing Aging Cells
Senolytics are the secret to reversing aging cells. This exciting treatment helps slow down the aging process, build health, and increase vitality.
Holistic Diabetes Treatment In Boca Raton
If you're searching for diabetes treatment in Boca Raton, visit a health care clinic that knows how to completely restore health.
5 Reasons Why You Need A Functional Medicine Coach
Are you having trouble reaching your health goals on your own? A functional medicine coach can help!
Boca Raton’s Holistic Wellness Center
Therefore, solutions to symptoms are carefully designed SPECIFICALLY for each person. As these combinations (and dosages) are not available commercially (the combinations are too specific), many of our medical solutions come from a highly trusted and reputable compounding pharmacy.
Any Questions?
There Are a Variety of Ways to Get in Touch. Contact Us Directly Via Email, Live Chat, Form Submission, SMS, and Whatsapp. We are Happy To Hear From You.